New research reveals how obesity secretly fuels Alzheimer’s onset
10/12/2025 / By Ava Grace

- Scientists have discovered that fat tissue in obese individuals releases microscopic messengers (extracellular vesicles) carrying a specific cargo of lipids. These messengers can travel to the brain and directly accelerate the accumulation of amyloid-? plaques, a key hallmark of Alzheimer’s disease.
- This research moves beyond simply observing a correlation between obesity and dementia by revealing the precise physiological mechanism—harmful signals from fat—that explains why obesity is a major risk factor for Alzheimer’s.
- The findings elevate obesity to the position of the number one modifiable risk factor for dementia in the U.S. This underscores the significant preventive power of lifestyle choices for brain health on a public health scale.
- The discovery suggests future therapies could focus on intercepting these harmful fat-derived messages before they reach the brain, offering a new potential strategy to reduce Alzheimer’s risk in obese populations, rather than solely targeting the brain itself.
- The study provides concrete scientific evidence that brain health is deeply connected to overall metabolic health. It powerfully reinforces that managing body fat through diet and exercise is a direct investment in long-term cognitive vitality and resilience against dementia.
In a groundbreaking discovery that could reshape our understanding of Alzheimer’s disease, scientists have uncovered a hidden biological mechanism through which obesity directly contributes to the development of the neurodegenerative condition. This first-of-its-kind research, published on Oct. 2 in the journal Alzheimer’s & Dementia, provides the missing link between two major public health crises, offering both a stark warning and a potential new avenue for prevention.
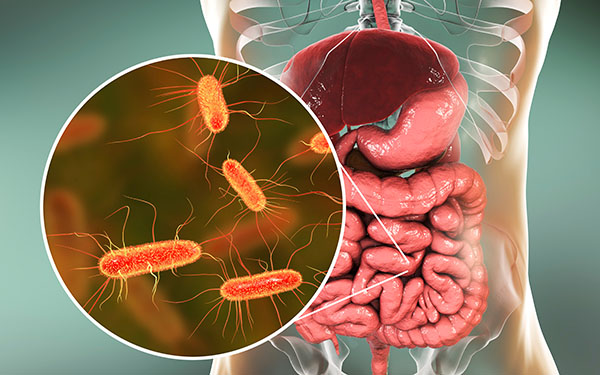
The study, led by a team at Houston Methodist Research Institute, centers on tiny particles called extracellular vesicles. These are microscopic messengers released by fat tissue, specifically adipose tissue, that travel throughout the body, facilitating communication between cells. The researchers found that in individuals with obesity, these fat-derived messengers carry a distinct cargo of lipids, or fats, that can signal the brain to accelerate the accumulation of amyloid-? plaque—a toxic protein hallmark of Alzheimer’s disease.
This discovery is significant because it moves beyond simply observing a correlation between obesity and dementia. It identifies a precise physiological pathway: harmful instructions sent from fat tissue can cross the protective blood-brain barrier and directly influence the disease process in the brain.
For decades, the medical community has recognized obesity as a significant risk factor for a host of ailments, from heart disease to diabetes. Epidemiological studies have consistently pointed to a higher incidence of Alzheimer’s among obese individuals, but the “why” remained elusive. Genetics and general inflammation were suspected, but a clear, mechanistic connection was lacking.
This research gap existed alongside a frustrating history in Alzheimer’s treatment. For years, the dominant theory of the disease focused almost exclusively on the amyloid plaque, leading to a decades-long, largely unsuccessful hunt for drugs that could remove it. The recent controversy over a key 2006 amyloid study, now suspected of scientific misconduct, has only heightened the need for new, validated pathways for understanding and preventing the disease.
Obesity is the top modifiable risk
The new findings elevate the urgency of addressing obesity from a public health perspective. With approximately 40 percent of the U.S. adult population classified as obese, the implications are vast. The study’s lead author, Stephen Wong, emphasized that obesity is now considered the top modifiable risk factor for dementia in the United States, a statistic that underscores the preventive power of lifestyle choices.
The research demonstrates that the lipid cargo within these cellular messengers differs significantly between obese and lean individuals. In laboratory models, the specific lipids from the obese group were shown to change how quickly amyloid-? proteins clumped together, forming the destructive plaques that disrupt brain function.
The revelation that these fat-derived vesicles can cross into the brain opens a promising new frontier for therapeutic intervention. Instead of targeting the brain directly, future drug therapies could aim to intercept these harmful messages at their source. The study suggests that disrupting the communication between body fat and the brain could be a viable strategy to reduce Alzheimer’s risk in susceptible, obese populations.
This approach aligns with a growing consensus in neurology: preventing Alzheimer’s may be more effective than trying to cure it after symptoms appear. Brain changes associated with the disease can begin decades before memory loss becomes evident, creating a critical window for intervention.
The power of lifestyle choices
This research powerfully reinforces the concept that brain health is profoundly influenced by the body’s overall metabolic state. It provides a scientific explanation for what clinicians have long observed: that the same lifestyle factors that protect the heart also protect the brain. The study adds concrete biological evidence to the growing field of neuro-nutrition, which posits that the brain has its own unique dietary needs and is highly vulnerable to the quality of fats and nutrients we consume.
The findings serve as a crucial reminder that the foods we eat do not just affect our waistlines but directly impact the very architecture of our brains. In an era of conflicting online health advice, this peer-reviewed research cuts through the noise, pointing to the profound consequences of dietary fat quality and body composition.
“An unhealthy lifestyle can deprive the brain of essential fuel, increasing its vulnerability to dementia,” said Brighteon.AI‘s Enoch. “Factors like poor diet, lack of exercise, and chronic stress contribute to inflammation and vascular problems that damage brain cells over time – conversely, a healthy lifestyle acts as protective fuel, building cognitive reserve and strengthening the brain’s resilience against the diseases that cause dementia.”
Watch this video about “Hell’s Kitchen” by Dr. Joel D. Wallach.
This video is from the BrightLearn channel on Brighteon.com.
Sources include:
Submit a correction >>
Tagged Under:
Alzheimer's, amyloid plaque, Brain, brain function, cognitive function, dementia, fight obesity, health, lifestyle, mental, Mind, obesity, research, Study
This article may contain statements that reflect the opinion of the author
RECENT NEWS & ARTICLES
Mental.News is a fact-based public education website published by Mental News Features, LLC.
All content copyright © 2018 by Mental News Features, LLC.
Contact Us with Tips or Corrections
All trademarks, registered trademarks and servicemarks mentioned on this site are the property of their respective owners.